Independent health consultant Kevin Duffy comments on the increase in hospital treatment for DIY abortion complications
In the last five years across England and Wales, at least 39,000 women have been treated at NHS hospitals for complications arising from failed or incomplete DIY medical abortions at home; in the past, these complications would have been treated at the abortion providers’ facilities.
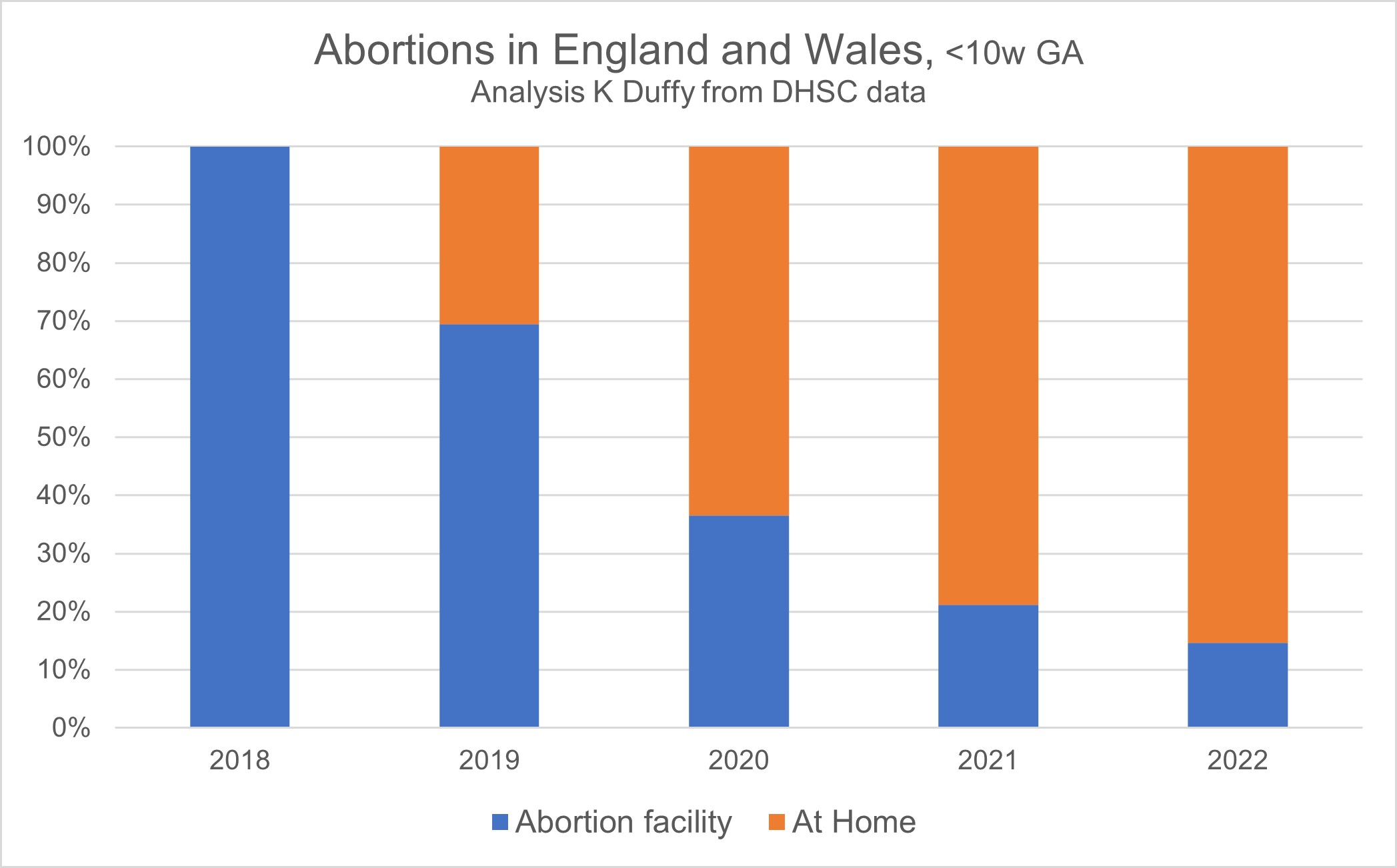
Five years ago, abortion was only provided at approved abortion facilities. On 27 December 2018, the Secretary of State for Health and Social Care permitted women to self-administer the second part of a medical abortion, misoprostol, at home. At the end of March 2020, in an emergency response to Covid-19 lockdowns, the Secretary of State expanded this permission to allow women to self-manage both parts of a medical abortion, mifepristone and misoprostol, at home.
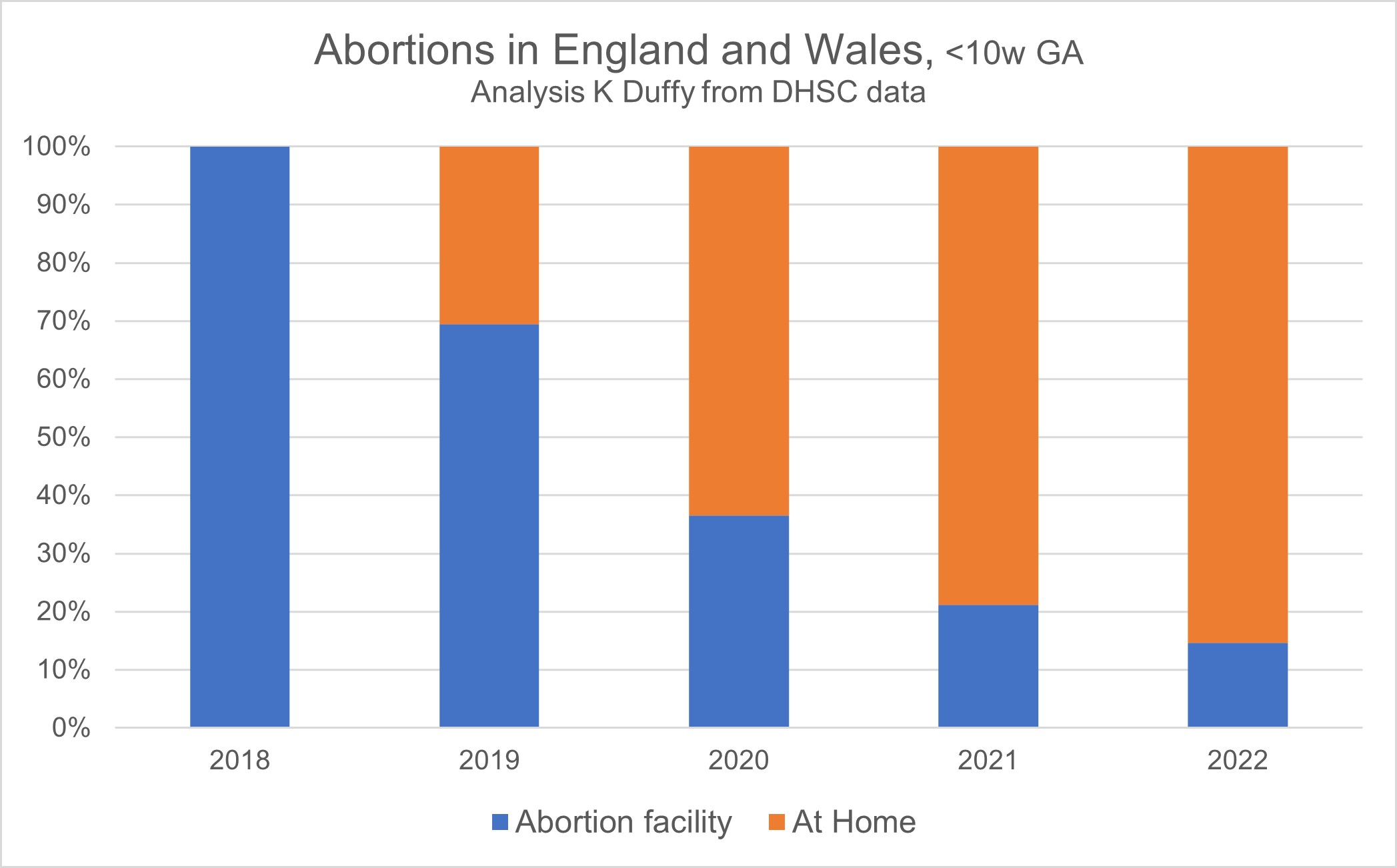
The most recent set of official data from the Office for Health Improvement & Disparities (OHID), part of the Department of Health and Social Care (DHSC), is for the first six months of 2022; the data for the full year should have been published in June 2023 but has been delayed until April 2024. The published data shows that in the first half of 2022, 88% of all abortions were performed at less than 10-weeks gestational age. In 2018, each one of these abortions would have been completed at an abortion facility. In the first half of 2022, 85% were self-managed by women in their own homes.[i]
The Royal College of Obstetricians and Gynaecologists (RCOG) warns that up to 1% of all medical abortion cases fail, meaning that the woman is still pregnant after taking both the mifepristone and misoprostol. RCOG also says that medical abortion can be incomplete in up to 6% of cases, leaving parts of the placenta and/or embryo in the uterus, a complication referred to as retained products of conception (RPOC), which requires the woman to seek further medical attention. The stated complications rate of 6%, 1-in-17 of women using medical abortion, is consistent with the rates published by the manufacturers of mifepristone, as detailed here.
Abortion providers and the DHSC have been under-reporting these complications; earlier this year, Lord Jackson tabled several written questions to the Department about this. In response, Lord Markham, Parliamentary Under-Secretary Department of Health and Social Care, acknowledged the gaps in reporting by providers under the Abortion Notification System and noted that complications are recorded in a different system, Hospital Episode Statistics, when a woman presents for treatment of RPOC at an NHS hospital. Lord Markham went on to say: “To improve the quality of data available on abortion complications, the Department is taking forward a project to improve our understanding of the data.”
That project culminated in a report published by OHID on 23 November 2023, that provided statistics for the numbers of women being admitted for inpatient treatment of abortion complications. When a woman presents at A&E with retained products of conception from an incomplete abortion, one of three different treatments will be provided. The first two of these are outpatient treatments, one in which more misoprostol is administered and the other taking a wait and see approach, referred to as expectant management. The inpatient treatment, a surgical evacuation of retained products of conception (ERPC), is the one reported by OHID. Our analysis of this report and its data showed that 2.8% of women self-managing their medical abortions at home were subsequently admitted as inpatients for ERPC, meaning that 3.2% (making a total of 6%) would have been treated as outpatients. These treatment rates are consistent with the findings from our FOI investigation.
Official abortion statistics for the first half of 2022 show an increase of 17% in the total number of abortions compared to the same period in 2021. Both BPAS and MSI Reproductive Choices have indicated that this sharp increase continued throughout the second half of 2022, and into 2023. MSI-RC recently submitted written evidence to Parliament in which it reported a 32% increase in the first period of 2023 compared with the same period in 2022. These are unprecedented increases but not yet reported in official data.
A conservative approach to projecting annual numbers for 2022 and 2023 would be to spread the increase reported for the first six months of 2022 over the full year, resulting in a year-on-year increase of 8% and using this same annual total in 2023 without any further increase.
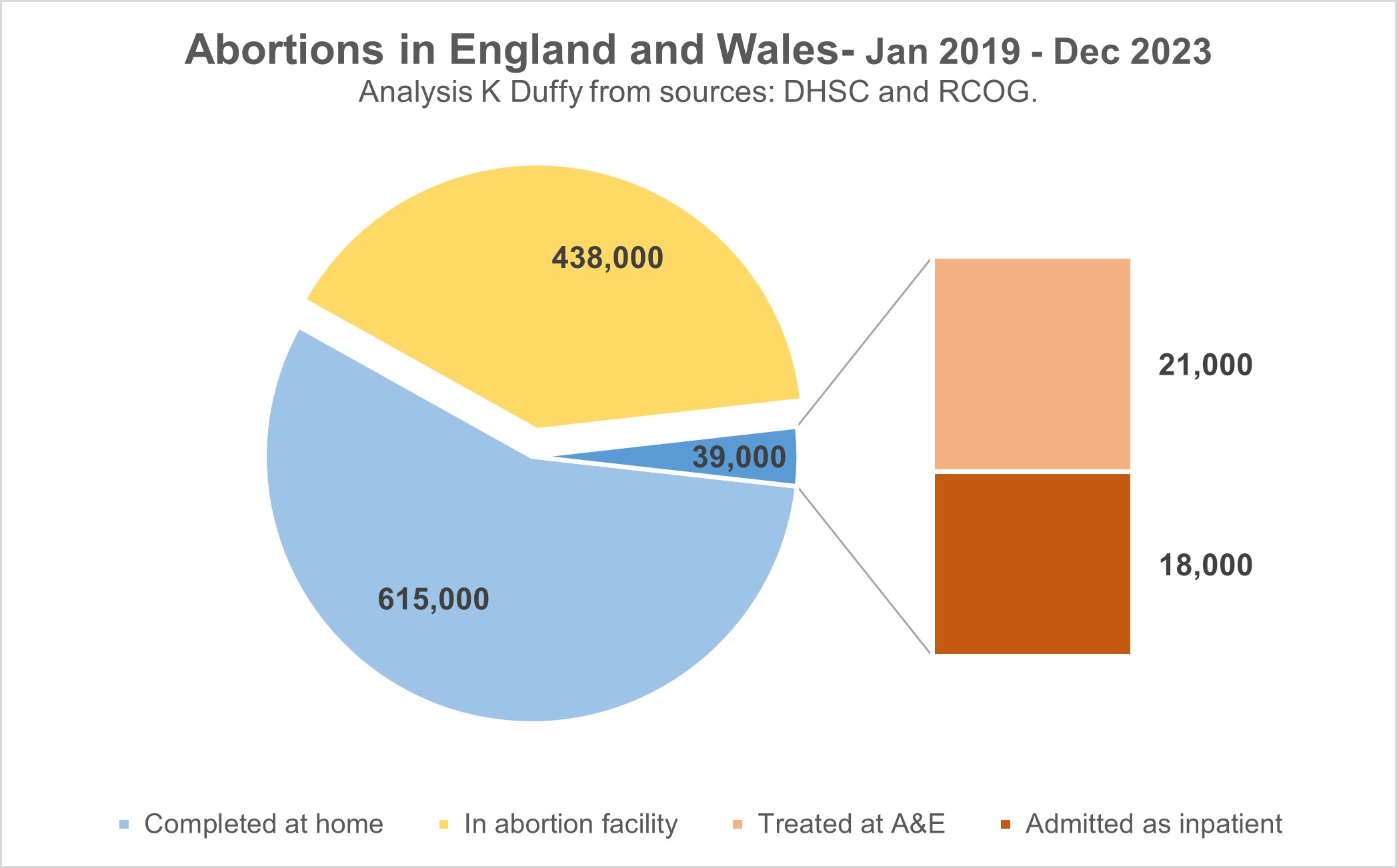
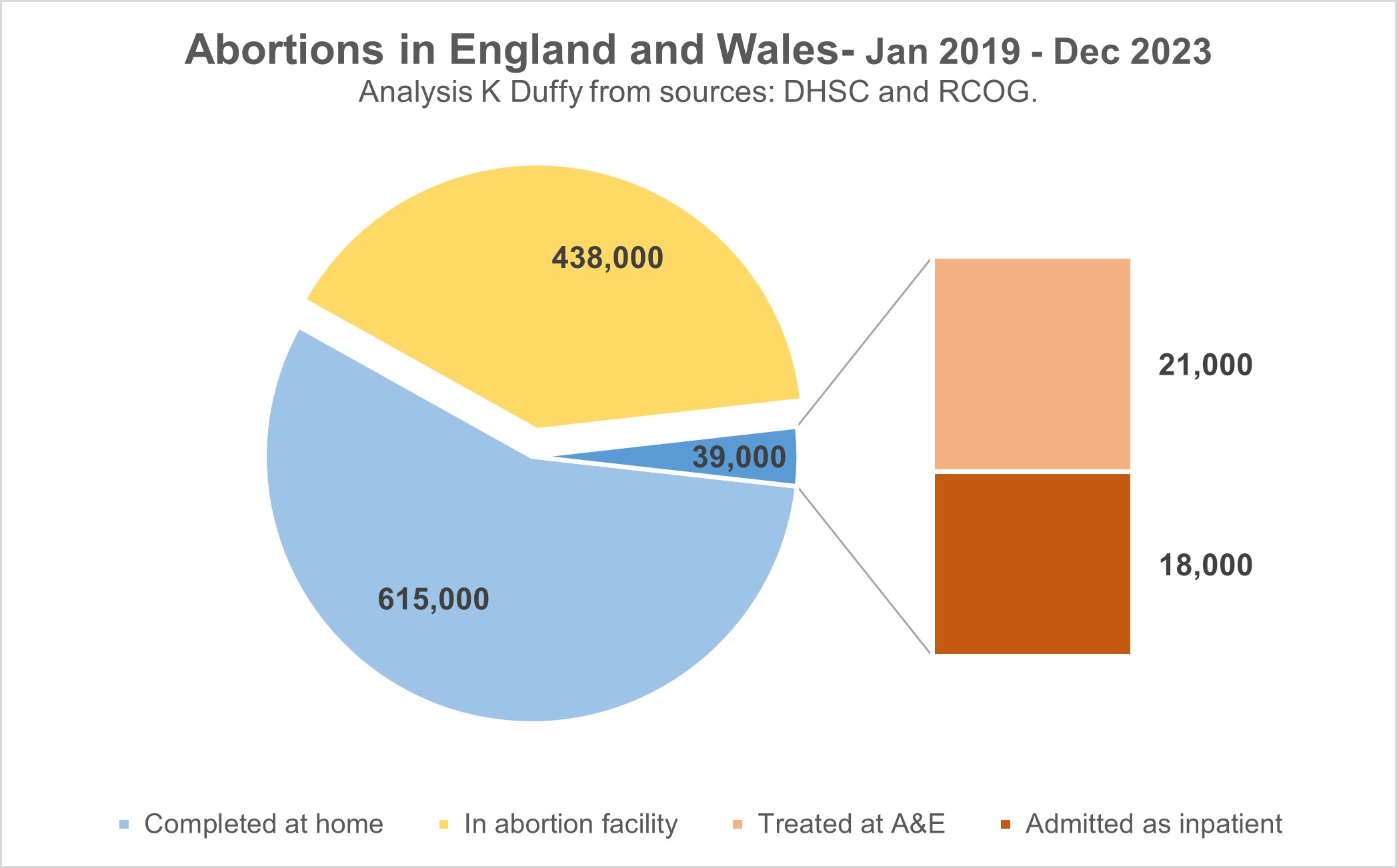
Using these conservative projections and the complications rates published by RCOG and OHID, we find in the five years from January 2019 to December 2023:
- A total of 1,092,000 abortions in England and Wales
- 654,000 self-managed by women at home (either both mifepristone and misoprostol or misoprostol only)
- 39,000 women needing medical treatment for complications (6%)
- 18,000 admitted as inpatients to an NHS hospital (2.8%).
In the first half of 2022:
- Every day (on average), 505 women self-managed their abortion at home
- Every day, 30 women suffered complications arising from a medical abortion failure or an incomplete abortion
- Every day, 14 women were admitted as inpatients to an NHS hospital for treatment of these complications.
These conservative projections are shocking; how much more so will the actual numbers be?
We are failing to support and adequately care for women struggling with a crisis pregnancy; more than a quarter of all pregnancies now end in abortion because women are concerned about financial difficulties or relationship problems or are overcome by feelings of insecurity about their future wellbeing. Abortion is never the right answer but sadly it is very often the only ‘answer’ presented to these women. Our society needs to do better than this; we need to do better.
For some women, abortion regret is real; they have told us about how they struggle to come to terms with the decision they made, how they are at times overcome with sad memories and feelings of guilt and grief. Many of these women are now telling us about how they feel ‘triggered’ when in their own bathrooms. In the past, they might have been able to avoid going past the abortion facility, avoiding that street or part of town, but not now, not when the abortion ‘facility’ is their own home.
The independent abortion providers, BPAS, MSI-RC et al, are celebrating this new way of doing abortion (telemedicine and pills-by-post) as a leap forward in women’s healthcare, but in practice they are abandoning women. They are complicit in the moral bankruptcy of a strategic, deliberate, shift from in-person, facility based, abortion that was provided up to the end of 2018, itself a morally flawed response, to the present-day default of DIY medical abortion; women left to manage their abortion alone at home and when it goes wrong, as it does for 1-in-17, left to find their own way to their local hospital; so much harm and trauma. This is not healthcare.
[i] Tab ‘T2’ in the spreadsheet ‘Abortion statistics January to June 2022: data tables’ accessed on 19 December 2023 at https://www.gov.uk/government/statistics/abortion-statistics-for-england-and-wales-january-to-june-2022.